Background: Acquired Hemophilia is a rare bleeding disorder characterized by the presence of autoantibodies (inhibitors) against coagulation factors, mainly targeting factor VIII. It predominantly affects older individuals with underlying autoimmune disorders or malignancies. Achieving hemostasis and inhibiting autoantibody production through immunosuppression are the mainstays of treatment. However, overcorrection of bleeding poses a risk of thrombosis, while immunosuppression increases the risk of infectious complications in older patients with co-existing comorbidities. This study sheds light on the epidemiology of acquired hemophilia, including readmission rates and causes of readmission.
Methods: We conducted a retrospective cohort study using the Nationwide Readmissions Database from 2016 to 2019 to identify hospitalizations with acquired hemophilia, using the ICD-10-CM (International Classification of Diseases, Tenth Revision, Clinical Modification) code D68.311. Descriptive analysis was performed to report patient demographics, hospital characteristics, various comorbid conditions, and complications. The all-cause 30-day readmission rate was calculated, excluding index admissions from December and deaths during index admissions. Additionally, primary diagnoses at readmission were identified. The analysis produced national estimates after applying weights, utilizing the methodology provided by the Healthcare Cost and Utilization Project.
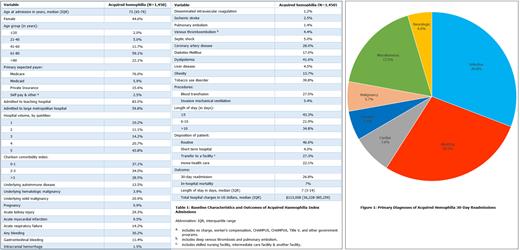
Results: Out of 1,450 admissions for acquired hemophilia between 2016 and 2019 in the United States, 803 (55.4%) were males, and 857 (59.1%) belonged to the age group of 61-80 years, with a median age at admission of 73 years. Furthermore, the majority were admitted to a teaching hospital (83.5%), with the highest quintile of acquired hemophilia-specific hospital volumes (43.8%) in a large metropolitan area with at least 1 million residents (59.8%). Although 20.9% had an underlying solid malignancy, only 28.5% had an otherwise high comorbidity burden with the Charlson comorbidity index of >3. Underlying hematologic malignancy was reported in 3.9% of admissions, and 13.5% had a diagnosis of an autoimmune disease. Regarding complications, acute myocardial infarction occurred in 9.5%, disseminated intravascular coagulation was noted in 1.2%, intracranial hemorrhage in 1.5%, ischemic stroke in 2.5%, and venous thromboembolism in 4.4%, with 30.2% of admissions experiencing some form of bleeding. The median length of stay was 7 days, and 101 deaths occurred during the index admission, resulting in a 7% inpatient mortality rate. Out of 1,349 patients who were discharged alive, 371 were readmitted within 30 days, with a 30-day readmission rate of 27% (table 1). The median time to readmission was 10 days (interquartile range 5-18), and the median length of stay during readmission was 7 days (interquartile range 3-14), with 10.8% mortality during readmission. The median hospitalization charges were $11,3008 for both index admissions and readmissions. After omitting readmissions coded as hemophilia, infection (30.8%), followed by bleeding (28.2%), was the most common cause for readmission (figure 1).
Conclusion: The study highlights a high rate of bleeding and thrombotic complications in acquired hemophilia, necessitating a careful approach to factor replacement for achieving hemostasis. Moreover, bleeding and infection are the primary reasons for the elevated 30-day readmission rate of 27%, and there is an additional 11% mortality during readmission, indicating a significant incidence of treatment-related toxicity and disease relapse.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal